When considering an "upper GI endoscopy" for a "95-year-old" with "dementia", many families find themselves seeking shared experiences and advice. This medical procedure, which allows doctors to examine the upper part of the gastrointestinal tract, can be particularly challenging for elderly patients due to their unique health concerns and cognitive impairments. In this article, we will explore what to expect from the procedure, potential risks, and tips for caregivers navigating this decision.
Upper GI endoscopy is often recommended for various reasons, including diagnosing conditions such as "gastroesophageal reflux disease (GERD)", ulcers, or other gastrointestinal issues. For older adults, especially those with dementia, the decision to proceed with an endoscopy can be complex. It is essential to weigh the benefits against the risks and to consider the patient's overall quality of life.
Understanding the Procedure
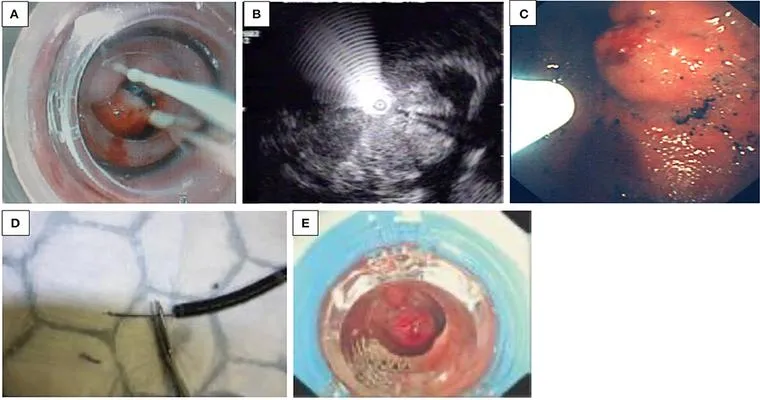
An "upper GI endoscopy" involves the use of a flexible tube with a camera, called an endoscope, which is inserted through the mouth and into the esophagus, stomach, and the first part of the small intestine. The procedure typically requires sedation, which can pose additional risks for elderly patients, particularly those with cognitive decline. Understanding the implications of sedation for someone with dementia is crucial, as it may lead to increased confusion or agitation after the procedure.
Risks and Considerations
For a "95-year-old" patient with "dementia", there are several factors to consider before proceeding with an upper GI endoscopy. These include:
1. "Sedation Risks": Older adults often have decreased physiological reserves, making them more susceptible to complications from sedation.
2. "Cognitive Effects": Post-procedure confusion or delirium can occur, particularly in patients with existing cognitive impairments.
3. "Invasion of Privacy": For patients with dementia, the invasiveness of the procedure can be distressing. It is essential to consider their comfort and mental state.
4. "Recovery Time": Recovery may take longer for elderly patients, requiring additional support and monitoring.
Preparing for the Procedure
If you decide to move forward with the upper GI endoscopy, preparation is key. Here are some tips to help ensure a smoother process:
"Consult with Healthcare Providers": Discuss all concerns with the healthcare team, including potential risks and benefits specific to the patient's condition.
"Post-Procedure Plans": Arrange for a caregiver or family member to be present after the procedure, as the patient may be disoriented or need assistance.
"Communicate Clearly": Prepare to explain the procedure to the patient in a way they can understand, even if their cognitive function is impaired.
Post-Procedure Care
After the "upper GI endoscopy", monitoring the patient's response to sedation is crucial. Look for signs of confusion, agitation, or changes in behavior. Providing a calm and familiar environment can help ease any post-procedure anxiety. Additionally, ensure that the patient stays hydrated and follows any dietary restrictions or recommendations given by the healthcare team.
Conclusion
Gathering experiences from others can be invaluable when making healthcare decisions for a "95-year-old" with "dementia". An "upper GI endoscopy" can provide critical insights into gastrointestinal health, but the unique challenges posed by both age and cognitive impairment must be carefully navigated. Always consult with medical professionals and consider the individual’s quality of life when making decisions about medical procedures. By staying informed and prepared, families can better support their loved ones through the complexities of healthcare in the later stages of life.