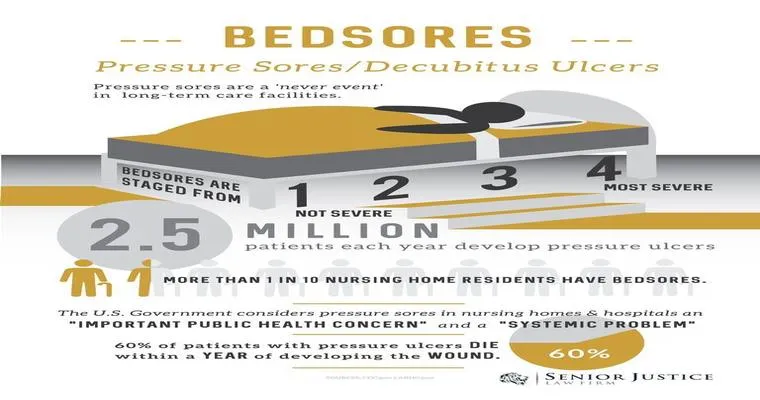
"Bedsores", also known as "pressure ulcers" or "decubitus ulcers", are a common and unfortunate consequence for individuals who are bedridden or have limited mobility. These painful sores develop when sustained pressure on the skin restricts blood flow, leading to tissue damage. Understanding the causes, prevention, and treatment of bedsores is crucial for caregivers and loved ones of those at risk.
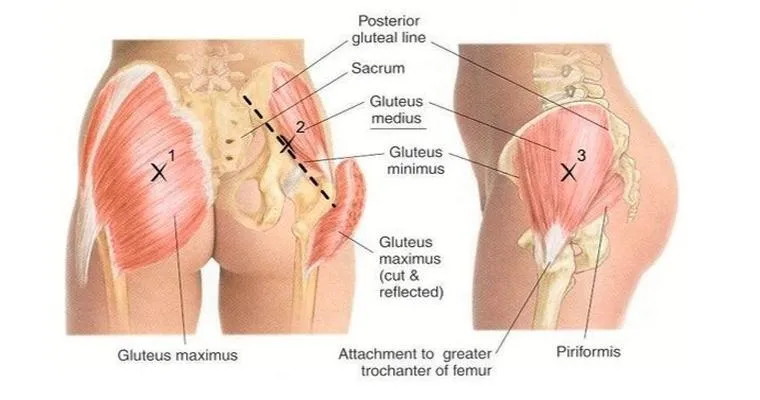
Bedsores typically form over bony areas of the body, such as the heels, elbows, hips, and tailbone. The risk of developing bedsores increases significantly for patients in hospitals, nursing homes, or those recovering at home after surgery or injury. Prolonged pressure, friction, and shear forces can all contribute to the formation of these ulcers. Therefore, it is essential to recognize the "inevitability" of bedsores in certain situations and take proactive measures to mitigate their impact.
Causes and Risk Factors
Several factors contribute to the development of bedsores. The primary cause is prolonged pressure on the skin, which can be exacerbated by other conditions such as:
1. "Limited Mobility": Individuals who cannot change positions independently are at a higher risk.
2. "Poor Nutrition": Malnutrition can weaken the skin and reduce its ability to heal.
3. "Moisture": Excess moisture from sweat or incontinence can lead to skin breakdown.
4. "Age": Older adults are more susceptible due to thinner skin and reduced blood flow.
Prevention Strategies
Preventing bedsores requires a comprehensive approach. Here are some effective strategies:
1. "Regular Position Changes": Encourage individuals to change their position at least every two hours to relieve pressure on vulnerable areas.
2. "Use of Support Surfaces": Specialized mattresses and cushions can help distribute weight evenly and reduce pressure points.
3. "Maintain Skin Hygiene": Keep the skin clean and dry to prevent moisture-related damage. Regular inspections of the skin can help detect early signs of bedsores.
4. "Adequate Nutrition and Hydration": A balanced diet rich in vitamins and minerals supports skin health and aids in healing.
Treatment Options
If bedsores do occur, prompt treatment is essential to prevent further complications. Treatment options may include:
1. "Wound Care": Cleaning the ulcer and applying appropriate dressings to promote healing and prevent infection.
2. "Debridement": In some cases, removing dead tissue from the sore may be necessary to facilitate healing.
3. "Pain Management": Providing relief through medications or topical treatments can improve the comfort of the affected individual.
4. "Surgical Intervention": Severe cases may require surgical procedures to close the wound or remove damaged tissue.
Conclusion
While the development of "bedsores" may seem inevitable in certain situations, understanding the risk factors and implementing preventive measures can significantly reduce their occurrence. Caregivers and family members play a vital role in monitoring at-risk individuals and ensuring proper care is provided. By prioritizing prevention and early intervention, the impact of bedsores can be minimized, leading to improved quality of life for those affected.