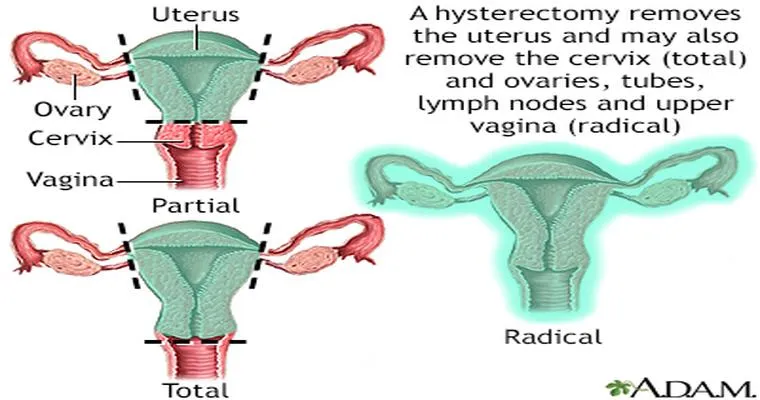
Experiencing "bleeding after a full hysterectomy", even years post-surgery, can be concerning for many women. A hysterectomy, which involves the removal of the uterus, is typically performed to address various medical conditions, including fibroids, endometriosis, or cancer. If you find yourself dealing with this unexpected symptom, it is essential to understand the potential causes and seek appropriate "medical advice".
Bleeding after a hysterectomy can stem from various factors. One possibility is the presence of "vaginal atrophy", which is a thinning and inflammation of the vaginal walls due to decreased estrogen levels. This condition is common in women who have undergone menopause, particularly those who have had their ovaries removed during the hysterectomy. It can lead to dryness and bleeding, often during intercourse or after physical activity.
Another potential cause of bleeding could be "granulation tissue". After surgery, the healing process can sometimes lead to the formation of this tissue, which is made up of new blood vessels and can be sensitive and bleed easily. This is generally not serious but can be uncomfortable and may require treatment.
In some cases, the bleeding might indicate a more serious issue, such as "pelvic organ prolapse" or even the recurrence of a condition that led to the hysterectomy. Therefore, it is crucial to monitor the bleeding's frequency and severity and to keep track of any accompanying symptoms, such as pain or unusual discharge.
If you are experiencing bleeding years after a full hysterectomy, here are some suggestions to consider:
1. "Consult Your Doctor": The first step should always be to talk to a healthcare professional. They can conduct a thorough examination, including a pelvic exam, and may recommend imaging tests to determine the cause of the bleeding.
2. "Hormonal Therapy": If vaginal atrophy is diagnosed, your doctor might suggest estrogen therapy, either in the form of vaginal creams, rings, or systemic hormone replacement therapy. This can help restore moisture and elasticity to the vaginal tissues.
3. "Lifestyle Modifications": Maintaining a healthy lifestyle can also aid in managing symptoms. Staying hydrated, using water-based lubricants during intercourse, and avoiding irritants can help reduce discomfort.
4. "Follow-Up Care": Regular check-ups with your gynecologist are essential, especially if you have a history of reproductive health issues. These visits can help catch any potential problems early.
5. "Seek Support": Joining a support group for women who have undergone hysterectomies can provide comfort and shared experiences. Hearing from others in similar situations can offer valuable insights and coping strategies.
In conclusion, while "bleeding after a full hysterectomy" years later can be alarming, it is important to remember that several factors may contribute to this symptom. By seeking professional medical advice and considering various management strategies, you can address the issue effectively and improve your quality of life. Remember, your health is paramount, and timely intervention is key to ensuring your well-being.