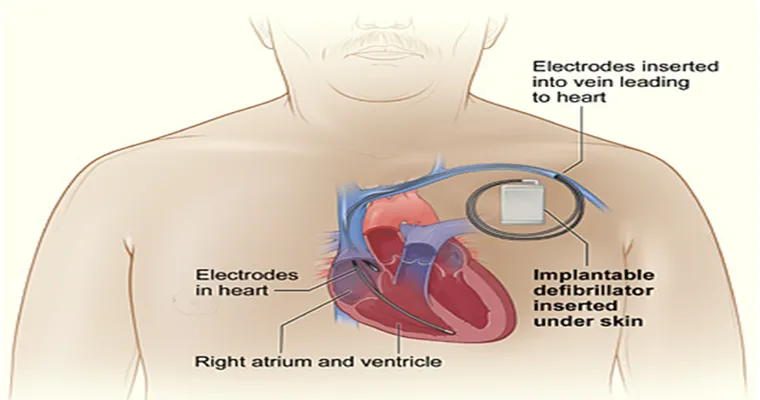
Making the decision to turn off an "ICD (Implanted Cardioverter Defibrillator)" for a loved one in "hospice care" can be an incredibly challenging and emotional experience for families. An ICD is a device that monitors heart rhythms and delivers shocks to restore a normal heartbeat if it detects a dangerous condition. While these devices can be life-saving, their purpose may shift once a patient enters hospice, where the focus is on comfort rather than curative treatment. This article explores the considerations and experiences families face when contemplating this significant decision.
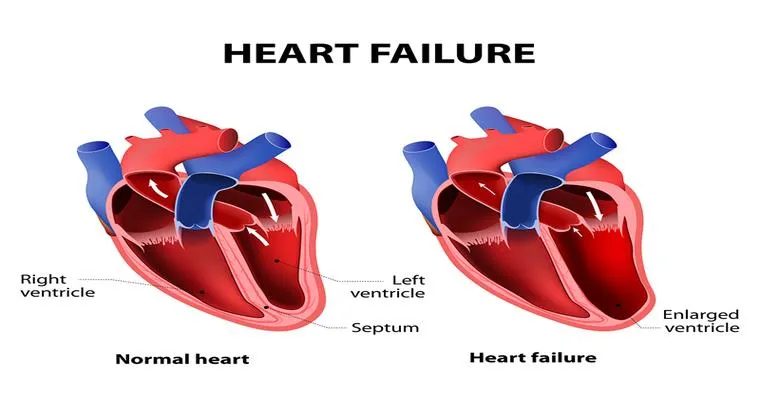
When someone is in hospice care, the primary goal is to ensure that the patient is comfortable and free from suffering. For many families, understanding the role of the ICD in this context is crucial. Patients may have lived with their ICD for years, relying on it to manage their heart conditions. However, as health declines and the focus turns to palliative care, the question arises: Is it time to turn off the ICD?
The decision to deactivate an ICD should involve thorough discussions with the healthcare team, including doctors, nurses, and hospice staff. These professionals can provide valuable insights into what turning off the device entails and how it may impact the patient’s quality of life. It is essential for families to understand that deactivating the ICD does not equate to giving up; instead, it is about prioritizing comfort and dignity during the end-of-life process.
Families often report feeling a mix of emotions when faced with this decision. Guilt, fear, and uncertainty can cloud judgment, making it challenging to choose the best course of action. For some, the thought of stopping a device that has provided life-saving interventions can be daunting. Yet, many families find solace in knowing that they are honoring their loved one’s wishes and prioritizing their comfort in their final days.
It is also important to consider the potential outcomes of keeping the ICD active versus turning it off. An active ICD may deliver shocks that can cause distress and discomfort to a patient who is nearing the end of life. Turning off the device may lead to a more peaceful transition, allowing the individual to pass away naturally, free from the anxiety of unexpected shocks.
In conclusion, the decision to turn off an ICD for a loved one in hospice care is deeply personal and often complex. Families should engage in open conversations with medical professionals and each other to navigate this challenging process. Ultimately, prioritizing the patient’s comfort and dignity can guide families toward a decision that aligns with their loved one’s values and wishes. Sharing experiences and seeking support from others who have faced similar situations can also provide comfort and guidance during this difficult time.