Congestive Heart Failure (CHF) is a serious condition that can significantly impact the overall health and quality of life of individuals, particularly vulnerable populations such as a "98 year old" in the "late stage dementia". Understanding the interplay between these two conditions is crucial for caregivers and healthcare providers. This article explores how CHF can affect a late stage dementia patient, including the symptoms, challenges, and management strategies.
Understanding CHF and Late Stage Dementia
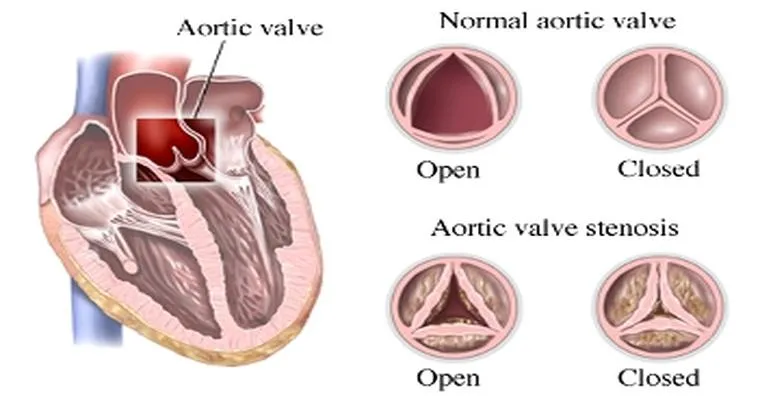
"Congestive Heart Failure" occurs when the heart is unable to pump blood effectively, leading to a buildup of fluid in the lungs and other body tissues. This condition can cause symptoms such as "shortness of breath", fatigue, and swelling in the legs and abdomen. On the other hand, "late stage dementia" is characterized by severe cognitive decline, where the individual may struggle with daily activities, communication, and recognition of loved ones.
The combination of these two conditions can lead to a complex clinical picture. Patients with late stage dementia may have difficulty expressing their discomfort or symptoms associated with CHF, making it challenging for caregivers to recognize and address their needs.
Symptoms and Challenges
For a "98 year old" patient with late stage dementia, the symptoms of CHF can manifest in several ways. These may include:
1. "Increased Confusion": Fluid buildup can lead to decreased oxygen levels, which may exacerbate cognitive decline and result in greater confusion or agitation.
2. "Decreased Mobility": Shortness of breath and fatigue can limit physical activity, further impacting the individual's overall health and ability to engage in daily life.
3. "Swelling and Discomfort": Edema in the legs and abdomen can cause discomfort, which may be difficult for a dementia patient to communicate.
4. "Changes in Appetite": CHF can lead to a loss of appetite or nausea, which can be particularly concerning for elderly patients who may already be at risk for malnutrition.
Management Strategies
Caring for a "98 year old" patient with late stage dementia and CHF requires a comprehensive approach. Here are some effective management strategies:
1. "Regular Monitoring": Caregivers should closely monitor the patient's weight, fluid intake, and any changes in mobility or cognitive function. Early detection of worsening symptoms can lead to timely interventions.
2. "Medication Management": It's essential to manage medications carefully, as some drugs may interact negatively with both dementia and heart failure treatments. Consulting with healthcare providers about any changes is crucial.
3. "Comfort Measures": Providing a comfortable environment can help ease symptoms. This may include using pillows for support, ensuring proper hydration, and managing any discomfort related to swelling.
4. "Communication": Caregivers should employ compassionate communication techniques, using simple and clear language. Non-verbal cues and reassuring touch can also help in alleviating anxiety or confusion.
5. "Palliative Care": In late stage dementia, focusing on the quality of life is paramount. Palliative care specialists can provide valuable support in managing symptoms and ensuring comfort for both the patient and their family.
Conclusion
CHF can profoundly affect a "98 year old" patient with "late stage dementia", leading to a unique set of challenges that require attentive care and management. By understanding the symptoms and implementing effective strategies, caregivers can help improve the patient's quality of life and ensure their comfort during this difficult time. Comprehensive care that addresses both conditions holistically is essential for providing the best possible support for these vulnerable individuals.