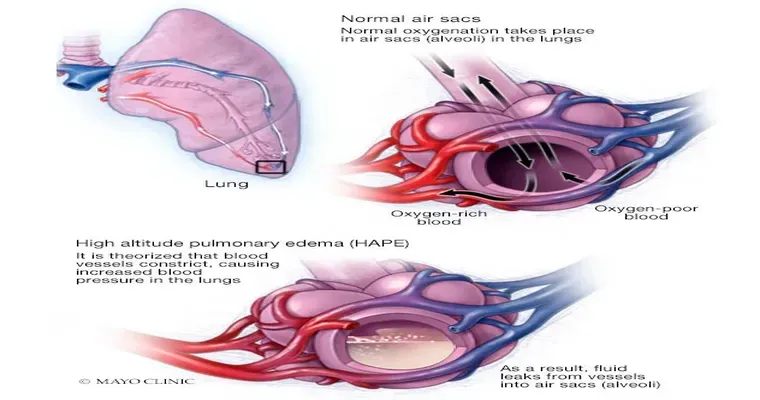
When caring for patients with "advanced dementia", it is not uncommon to encounter complications such as "pulmonary edema", which refers to the accumulation of "fluid in the lungs". This condition can significantly impact the patient's quality of life and may pose additional challenges for caregivers and healthcare providers. Understanding the relationship between dementia and pulmonary edema is crucial for providing appropriate care and support. In this article, we will explore the experiences of caregivers and healthcare professionals dealing with this complex situation and share insights on management strategies.
Understanding Pulmonary Edema in Dementia Patients
Patients with advanced dementia often experience a decline in their overall health, making them susceptible to various medical issues, including "pulmonary edema". This condition can arise from several factors, including heart failure, infections, or complications related to immobility. In patients with dementia, the inability to communicate discomfort or changes in their health can complicate the early detection of pulmonary edema.
Symptoms and Diagnosis
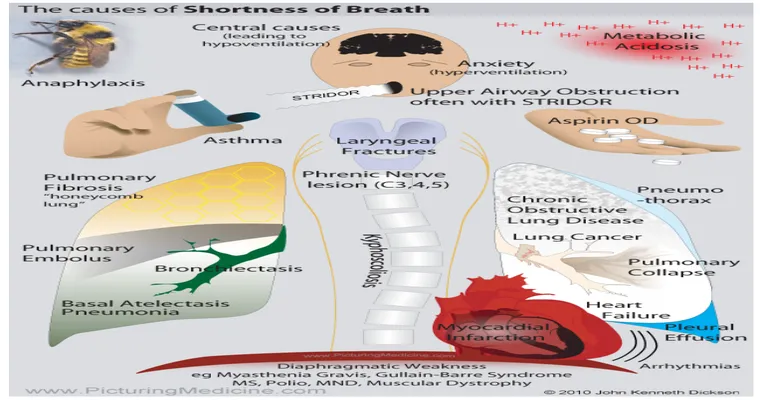
Recognizing the symptoms of pulmonary edema in patients with dementia can be challenging. Common signs include "shortness of breath", coughing, wheezing, and an increased respiratory rate. Caregivers should also be vigilant for changes in behavior, as patients may become more agitated or restless due to difficulty breathing. A thorough assessment by a healthcare professional is essential in diagnosing pulmonary edema, which may involve physical examinations, imaging studies, and laboratory tests.
Management Approaches
Managing pulmonary edema in patients with advanced dementia requires a multifaceted approach. Here are some strategies based on the experiences of caregivers and healthcare professionals:
1. "Monitoring Respiratory Function": Regular assessments of respiratory function can help detect early signs of pulmonary edema. Keeping a close eye on oxygen saturation levels and respiratory patterns is essential.
2. "Medication Management": Diuretics are often prescribed to help reduce fluid accumulation in the lungs. Caregivers should work closely with healthcare providers to ensure that medications are administered correctly and monitor for any side effects.
3. "Positioning": Elevating the head of the bed can help improve breathing and reduce discomfort. Caregivers should consider using pillows or specialized beds to assist with positioning.
4. "Palliative Care": In advanced stages of dementia, the focus may shift toward palliative care, which emphasizes comfort rather than curative treatment. Caregivers should discuss options with healthcare providers to ensure the patient’s dignity and quality of life are maintained.
5. "Support for Caregivers": Caring for a patient with advanced dementia and pulmonary edema can be emotionally and physically taxing. Caregivers should seek support from healthcare teams, support groups, or counseling services to manage stress and maintain their own well-being.
Conclusion
The interplay between "pulmonary edema" and "advanced dementia" presents unique challenges for both patients and caregivers. Sharing experiences and strategies can provide valuable insights into managing this complex condition. If you have encountered similar situations or have advice on coping with pulmonary edema in dementia patients, your contributions could greatly benefit others in the caregiving community. Understanding and addressing these challenges can lead to improved care and a better quality of life for patients suffering from these conditions.