Alzheimer’s Disease is a progressive neurological disorder that affects memory, thinking, and behavior. Early "diagnosis" is crucial for effective management and treatment of the condition. Various "medical tests" are employed to diagnose Alzheimer’s Disease, enabling healthcare professionals to differentiate it from other types of dementia and cognitive impairments. Understanding these diagnostic tools can help patients and families navigate the complexities of this condition.
The first step in the "diagnostic process" typically involves a thorough "medical history" and a physical examination. This helps to rule out other potential causes of cognitive decline. During this assessment, healthcare providers will ask about symptoms, family history, and any changes in behavior or daily functioning. It is essential for patients to provide comprehensive information to assist in making an accurate diagnosis.
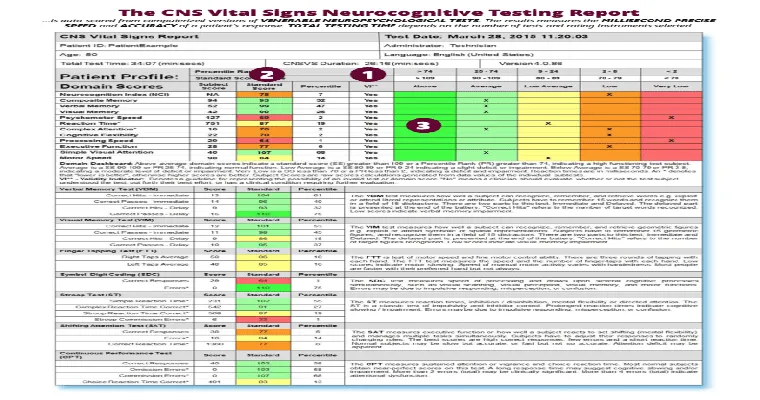
One of the core components of diagnosing Alzheimer’s Disease is "cognitive testing". This involves a series of standardized tests designed to assess memory, problem-solving abilities, attention, and language skills. The "Mini-Mental State Examination (MMSE)" and the "Montreal Cognitive Assessment (MoCA)" are commonly used tools that can help identify cognitive impairment. These tests allow healthcare professionals to determine the extent of cognitive decline and monitor changes over time.
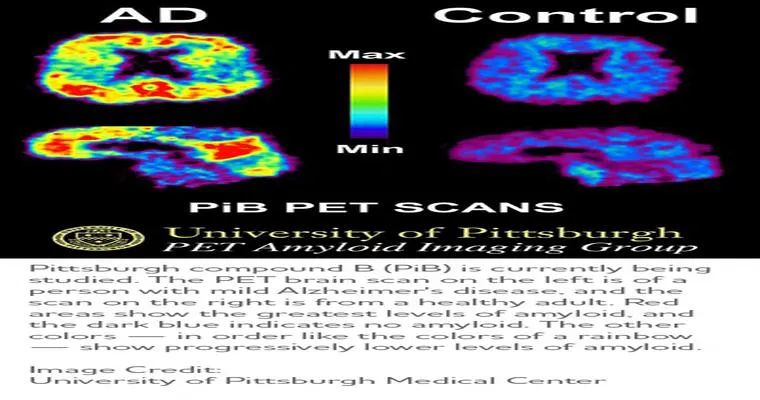
In addition to cognitive testing, healthcare providers may recommend "neuroimaging" studies. Techniques like "MRI (Magnetic Resonance Imaging)" and "CT (Computed Tomography)" scans can help visualize brain structure and identify any abnormalities. These imaging tests are particularly useful in ruling out other conditions, such as tumors or strokes, that may contribute to cognitive symptoms. More advanced imaging techniques, like "PET (Positron Emission Tomography)" scans, can detect amyloid plaques and tau tangles, which are characteristic of Alzheimer’s Disease.
Another important diagnostic tool is "laboratory tests". Blood tests can help identify other potential causes of cognitive decline, such as vitamin deficiencies or thyroid disorders. While there are currently no definitive blood tests for Alzheimer’s Disease, researchers are continually exploring biomarkers that may aid in diagnosis.
In some cases, "genetic testing" may be considered, particularly for individuals with a family history of Alzheimer’s. Tests for genes such as APOE-e4 can provide insight into a person’s risk of developing the disease, although having these genes does not guarantee that an individual will develop Alzheimer’s.
Finally, an "autopsy" remains the most definitive way to confirm a diagnosis of Alzheimer’s Disease, as it allows for the examination of brain tissue for the presence of amyloid plaques and tau tangles. However, this method is not practical for real-time diagnosis and is typically conducted post-mortem.
In conclusion, diagnosing Alzheimer’s Disease relies on a combination of "medical history", "cognitive testing", "neuroimaging", "laboratory tests", and, in some cases, "genetic testing". Early detection through these medical tests is essential for managing symptoms and planning for the future. If you or a loved one are experiencing signs of cognitive decline, it is crucial to consult with a healthcare professional who can guide you through the diagnostic process and available treatment options.