In the intricate realm of mental health, the distinction between "delusions" and "hallucinations" often sparks curiosity and confusion. For many, like my mom, recalling her "delusions" while overlooking her "hallucinations" raises an intriguing question: Do these experiences originate from different parts of the brain? Understanding these phenomena can shed light on the complexities of our mental processes and their neurological underpinnings.
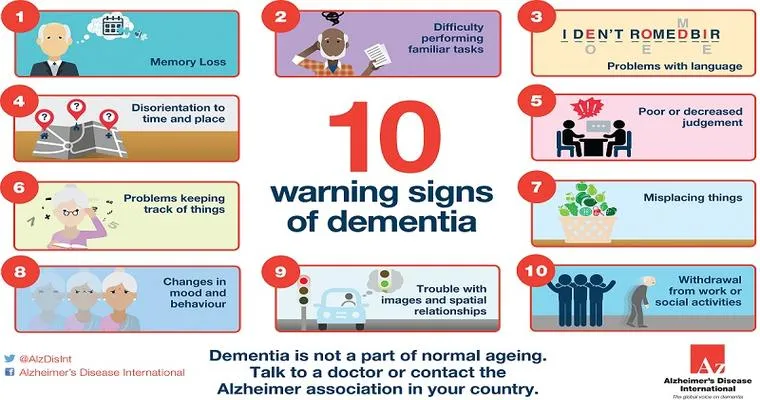
Delusions are false beliefs that persist despite evidence to the contrary. They can manifest in various ways, from believing that one has special powers to thinking that one is being persecuted. On the other hand, hallucinations involve perceiving things that are not present, such as hearing voices or seeing things that others do not. Both delusions and hallucinations are commonly associated with mental health disorders, including schizophrenia and bipolar disorder.
Research suggests that delusions and hallucinations may indeed engage different neurological pathways. Studies indicate that delusions may be linked to areas of the brain responsible for reasoning, belief formation, and cognitive processing. The prefrontal cortex, which plays a crucial role in decision-making and social behavior, is often implicated in the development of delusional thoughts. In contrast, hallucinations are typically associated with sensory processing regions, such as the temporal lobe, which is involved in hearing and visual perception.
The mechanisms that lead to these divergent experiences might also reflect underlying neurochemical differences. For instance, imbalances in neurotransmitters like dopamine and serotonin can contribute to both delusions and hallucinations, but their effects may vary based on the specific brain regions involved. This could explain why some individuals, like my mom, may vividly remember their delusional thoughts while having little or no recollection of their hallucinations.
Understanding the brain’s role in these phenomena can also enhance treatment approaches. Therapies targeting specific brain functions may help individuals manage their symptoms more effectively. Cognitive-behavioral therapy, for example, can assist those struggling with delusions by challenging and reframing their false beliefs. Meanwhile, antipsychotic medications are often prescribed to reduce both delusions and hallucinations, targeting the neurotransmitter imbalances that may underlie these conditions.
Moreover, the subjective experience of remembering delusions but forgetting hallucinations raises important questions about memory and perception. Memory is a complex process that involves encoding, storage, and retrieval of information. Different types of memory, such as episodic and semantic memory, may contribute to how individuals recall their experiences. This distinction might help explain why some aspects of mental health experiences are more memorable than others.
In conclusion, the relationship between "delusions" and "hallucinations" is a fascinating area of study that touches on both psychology and neuroscience. While my mom’s memories of her delusions linger, her forgetfulness about her hallucinations invites further exploration into the brain’s intricate workings. As research continues to evolve, we may gain deeper insights into how these distinct mental experiences arise from different regions of the brain, ultimately improving our understanding and treatment of mental health disorders. Engaging with these concepts not only enriches our knowledge but also fosters empathy for those navigating the complexities of their mental health journeys.