Experiencing "opposite changes in taste and smell" can be a perplexing issue, especially when combined with medical conditions like "Mild Cognitive Impairment (MCI)", "Frontotemporal Dementia (FTD)", and "heart failure". Understanding the possible connections between these symptoms and underlying health concerns is essential for caregivers and healthcare providers alike.
When individuals with MCI or FTD report changes in their sensory perceptions, it may indicate a deeper neurological issue. MCI is often considered a precursor to more severe forms of dementia, leading to difficulties in memory, thinking, and even sensory experiences. FTD, on the other hand, primarily affects behavior and language but can also alter how a person perceives taste and smell.
Heart failure, particularly when it affects both sides of the heart, can lead to reduced blood flow and oxygen to various organs, including the brain. This compromised circulation may contribute to neurological symptoms, including alterations in taste and smell. Research suggests that changes in these senses can also be linked to the medications used to treat heart failure, which may have side effects affecting taste and smell.
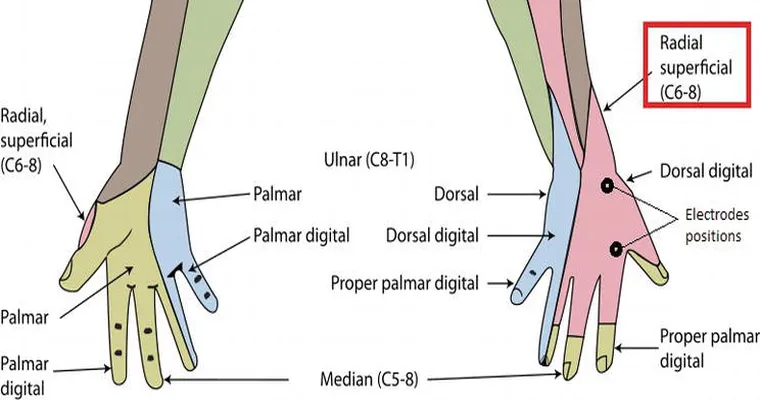
Moreover, the brain's regions responsible for processing taste and smell can be impacted by neurodegenerative diseases like MCI and FTD. The olfactory bulb, which plays a critical role in the sense of smell, can shrink in these conditions, leading to altered perceptions. This may explain why a person experiences opposite changes in taste and smell; one sense may become heightened while the other diminishes.
In addition to these factors, it is essential to consider lifestyle changes and nutritional status. Those with heart failure may experience changes in appetite or dietary choices, which could further influence taste sensations. If a person is not consuming a balanced diet, nutritional deficiencies can also lead to changes in sensory perceptions.
To address these issues, healthcare providers may recommend a comprehensive evaluation. This can include cognitive assessments, neurological examinations, and possibly adjustments in medication. Understanding the full scope of an individual's symptoms is crucial for developing an effective treatment plan.
In conclusion, opposite changes in taste and smell in a person experiencing MCI, FTD, and heart failure could be attributed to a combination of neurological decline, medication effects, and lifestyle factors. Caregivers should closely monitor these changes and seek professional guidance to support the individual’s overall well-being. By addressing the multifaceted nature of these symptoms, a more comprehensive approach to care can be implemented, enhancing the quality of life for those affected.