Navigating "Medicare coverage" can be a daunting task for many seniors and their families, especially when it comes to understanding the intricacies of "skilled nursing facility stays". As individuals age, the need for "rehabilitation services" often increases due to various health issues or recovery from surgery. Knowing how Medicare covers these services is crucial in ensuring that seniors receive the care they need without incurring overwhelming costs.
Understanding Medicare Coverage
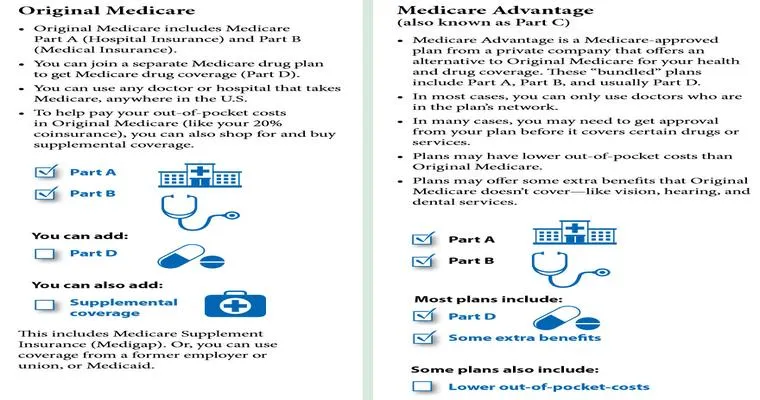
Medicare is divided into different parts, each covering specific services. For skilled nursing facility stays, most coverage falls under "Medicare Part A". This part is designed to help with inpatient hospital care, skilled nursing care, hospice, and some home health services. To qualify for coverage of a skilled nursing facility, patients must meet certain criteria outlined by Medicare.
Eligibility Criteria for Skilled Nursing Facility Coverage
To be eligible for "Medicare coverage" of a skilled nursing facility stay, the patient must have:
1. "A three-day inpatient hospital stay": Before being admitted to a skilled nursing facility, the patient must have been in a hospital for at least three consecutive days. This stay should be for a condition that requires skilled nursing care.
2. "A doctor’s recommendation": A physician must certify that the patient needs skilled nursing care or rehabilitation services on a daily basis.
3. "Care related to the hospital stay": The care provided in the skilled nursing facility must be for a condition that arose during the hospital stay or a condition that arose while receiving care for a related medical issue.
Coverage Details
Once these criteria are met, Medicare will cover the following:
"First 20 days": Medicare will cover the entire cost of a skilled nursing facility stay for the first 20 days. Patients have zero out-of-pocket costs during this period.
"Days 21 to 100": For days 21 to 100, Medicare requires a copayment. As of 2023, this copayment is approximately $200 per day. It is important to check for any annual updates as these amounts can change.
"Beyond 100 days": After 100 days, Medicare does not cover any costs associated with the skilled nursing facility stay. Patients will need to explore other insurance options or pay out-of-pocket.
Additional Considerations
Not all skilled nursing facilities are created equal. It is essential for seniors and their families to choose a facility that is certified by Medicare. To locate a certified facility, you can use the "Medicare Facility Locator" tool available on the official Medicare website.
In addition, families should inquire about the services offered at the facility, including physical therapy, occupational therapy, and speech therapy, to ensure that all rehabilitation needs are met.
Conclusion
Understanding "Medicare coverage" for skilled nursing facility stays is vital for seniors seeking rehabilitation services. By meeting the eligibility criteria and being aware of the coverage details, families can make informed decisions about care options. With the right knowledge, seniors can access the rehabilitation services they need while minimizing financial burdens. Always consult with a Medicare representative or a healthcare professional to get personalized advice tailored to individual circumstances.