Sundowning is a common phenomenon experienced by many "dementia patients", characterized by increased confusion, agitation, and emotional distress as the day transitions into night. This behavior can be challenging for both caregivers and loved ones, leading to heightened stress and anxiety. Understanding the causes of "sundowning" and implementing effective strategies to "minimize its effects" can significantly improve the quality of life for both patients and caregivers.
What Causes Sundowning?
The exact cause of sundowning is not fully understood, but several factors can contribute to its occurrence. As daylight fades, changes in "lighting" and "environmental cues" can disorient dementia patients, leading to increased confusion. Fatigue from a long day, coupled with the natural changes in the brain associated with dementia, can exacerbate these feelings. Additionally, unmet needs, such as hunger or discomfort, can lead to heightened agitation during these evening hours.
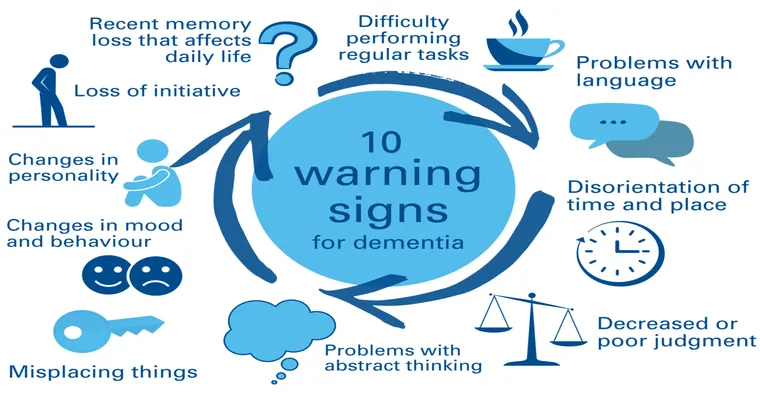
Signs and Symptoms of Sundowning
Recognizing the signs of sundowning is crucial for caregivers. Common symptoms include:
Increased "confusion" or disorientation
Heightened "irritability" or agitation
Restlessness or pacing
Difficulty in communicating
Mood swings or emotional outbursts
Identifying these symptoms early can help caregivers respond promptly and effectively.
Strategies to Minimize Sundowning
1. "Establish a Routine": Creating a consistent daily schedule can help dementia patients feel more secure and reduce anxiety. Regular meal times, activities, and bedtime can provide a sense of stability.
2. "Optimize Lighting": Bright, natural light during the day can help regulate the patient’s circadian rhythms. As evening approaches, gradually dimming the lights can create a calming atmosphere that signals it’s time to wind down.
3. "Engage in Activities": Encourage engaging and stimulating activities during the day to help reduce fatigue in the evening. Gentle exercise, such as walking or stretching, can also be beneficial.
4. "Monitor Nutrition": Ensure that dementia patients have balanced meals throughout the day. Avoid heavy meals late in the evening, as these can lead to discomfort and increased agitation.
5. "Create a Calm Environment": Reduce background noise and distractions in the evening. Playing soft music or engaging in quiet activities can promote relaxation and help ease the transition to nighttime.
6. "Use Comfort Items": Familiar items, such as favorite blankets or photographs, can provide comfort and reassurance during periods of confusion.
7. "Stay Calm and Reassuring": If a patient exhibits signs of sundowning, respond with calmness. Offer reassurance and gentle guidance, and avoid confrontation to prevent escalating the situation.
Conclusion
Understanding and managing sundowning in dementia patients is essential for enhancing their well-being and supporting caregivers. By recognizing the signs, implementing effective strategies, and fostering a calming environment, caregivers can significantly reduce the impact of sundowning. This proactive approach not only improves the quality of life for dementia patients but also alleviates stress for everyone involved, creating a more harmonious living situation.
With patience and understanding, caregivers can navigate the challenges of sundowning, ensuring that their loved ones feel safer and more secure during the evening hours.