As a caregiver, understanding "C. difficile" is crucial for maintaining the health and safety of those in your care. "Clostridium difficile", commonly referred to as C. difficile or C. diff, is a bacterium that can lead to severe gastrointestinal issues, particularly in vulnerable populations such as the elderly or those with weakened immune systems. This article will delve into the symptoms, causes, prevention, and treatment of C. difficile infections, providing caregivers with the knowledge needed to safeguard their patients.
Understanding C. Difficile
C. difficile is a spore-forming bacterium that can disrupt the normal balance of bacteria in the intestines. It is commonly associated with antibiotic use, which can kill off beneficial bacteria and allow C. difficile to thrive. Symptoms of a C. difficile infection can range from mild diarrhea to severe colitis, which can be life-threatening if not treated promptly. Caregivers should be vigilant for signs of infection, including:
Frequent, watery diarrhea
Abdominal pain or cramping
Fever
Nausea
Loss of appetite
Causes and Risk Factors
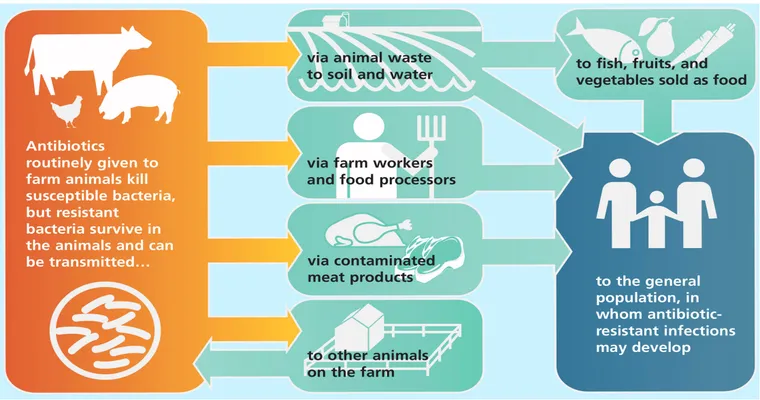
C. difficile infections are often linked to recent antibiotic use, but other factors can increase the risk as well. These include advanced age, prolonged hospital stays, and underlying health conditions. Caregivers should be aware that "C. difficile" can spread easily in healthcare settings, making it essential to follow strict hygiene practices.
Prevention Strategies
Preventing C. difficile infections starts with good hygiene. Here are some effective strategies caregivers can implement:
1. "Hand Hygiene": Regular handwashing with soap and water is critical, especially after using the restroom or handling contaminated items. Alcohol-based hand sanitizers are less effective against C. difficile spores.
2. "Cleaning and Disinfecting": Regularly clean and disinfect surfaces in patient care areas, particularly those that are frequently touched, such as doorknobs, bedrails, and medical equipment. Use EPA-approved disinfectants that are effective against C. difficile spores.
3. "Judicious Use of Antibiotics": Caregivers should work closely with healthcare providers to ensure that antibiotics are prescribed only when necessary, as overuse can disrupt gut flora and increase the risk of infection.
4. "Isolation Precautions": If a patient is diagnosed with a C. difficile infection, it is important to implement isolation precautions to prevent the spread of the bacteria to other patients.
Treatment Options
If a C. difficile infection is suspected, prompt medical attention is essential. Treatment typically involves:
"Antibiotics": Specific antibiotics, such as vancomycin or fidaxomicin, are prescribed to help eliminate the infection.
"Probiotics": In some cases, probiotics may be recommended to help restore the natural balance of gut bacteria.
"Fecal Microbiota Transplantation (FMT)": For recurrent infections, FMT can be considered, which involves transplanting healthy gut bacteria from a donor to restore balance.
Conclusion
C. difficile is a significant concern for caregivers, particularly in healthcare settings. By understanding the symptoms, causes, and preventive measures associated with "C. difficile", caregivers can play a vital role in protecting their patients from this potentially life-threatening infection. Always stay informed and collaborate with healthcare professionals to ensure the best care practices are being followed. Remember, your vigilance and knowledge are key in combating C. difficile effectively.