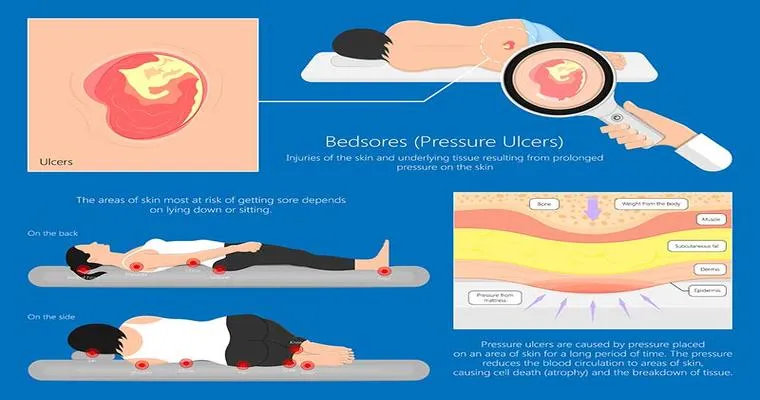
As a caregiver, understanding "bed sores", also known as "pressure ulcers" or "decubitus ulcers", is essential for providing the best possible care to those who are immobile or have limited mobility. Bed sores occur when there is prolonged pressure on the skin, often in areas where bones are close to the skin's surface, leading to "skin damage" and discomfort. This article will explore the causes, prevention, and treatment of bed sores, equipping you with the knowledge needed to protect your loved ones or patients effectively.
Understanding the Causes of Bed Sores
Bed sores develop when there is sustained pressure on the skin that restricts blood flow to the area. This can happen in various scenarios, including:
Prolonged immobility: Individuals who are bedridden or confined to a wheelchair are particularly at risk.
Friction and shear: Sliding down in bed or being moved roughly can cause skin abrasions, increasing the likelihood of bed sores.
Moisture: Excess moisture from sweating or incontinence can weaken the skin, making it more susceptible to damage.
Identifying the Risk Factors
Certain individuals are at a higher risk of developing bed sores. Key risk factors include:
Age: Older adults have thinner skin and decreased circulation, making them more vulnerable.
Medical conditions: Conditions such as diabetes, vascular disease, and neurological disorders can impair blood flow and sensation.
Nutrition: Poor nutrition and hydration can weaken the skin and hinder healing.
Prevention Strategies for Caregivers
Preventing bed sores is a crucial aspect of caregiving. Here are effective strategies caregivers should implement:
1. "Regular repositioning": Change the position of the individual at least every two hours to relieve pressure on vulnerable areas.
2. "Use pressure-relieving devices": Invest in specialized mattresses, cushions, and pads designed to reduce pressure on the skin.
3. "Maintain skin hygiene": Keep the skin clean and dry to prevent moisture from causing skin breakdown.
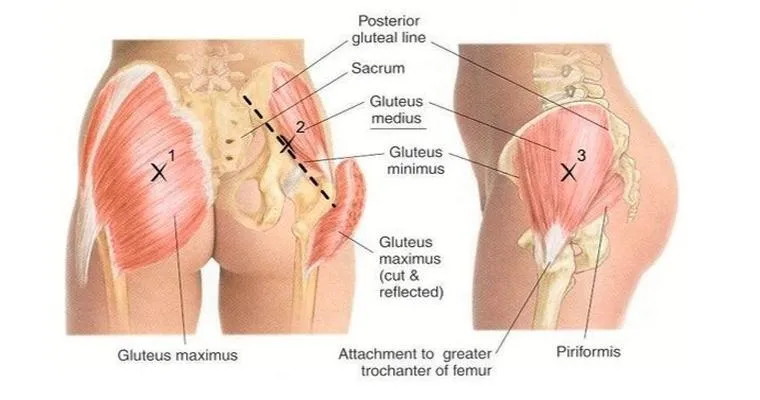
4. "Monitor skin condition": Regularly check for any signs of redness or skin breakdown, especially in bony areas like the heels, elbows, and tailbone.
5. "Encourage mobility": If possible, assist the individual in moving or encourage them to engage in physical activity to promote circulation.
Recognizing the Stages of Bed Sores
Bed sores are classified into four stages, each indicating the severity of the injury:
"Stage 1": The skin appears red and does not blanch when pressed. There may be discomfort in the affected area.
"Stage 2": The skin breaks open, forming a shallow ulcer that may look like a blister or abrasion.
"Stage 3": The sore extends deeper into the skin, potentially exposing fat tissue. The wound may appear crater-like.
"Stage 4": The pressure ulcer is severe, exposing muscle, bone, or tendons. This stage often involves significant tissue loss and can lead to serious infections.
Treatment Options for Bed Sores
If a bed sore does develop, prompt treatment is essential to prevent complications. Key treatment options include:
"Cleaning the wound": Gently clean the sore with saline or a mild soap solution to remove debris and bacteria.
"Applying dressings": Use appropriate dressings to keep the wound moist and protected from further injury.
"Managing pain and infection": Consult a healthcare provider for pain management and antibiotics if there are signs of infection.
"Nutritional support": Ensure adequate nutrition and hydration to promote healing.
Conclusion
Understanding "bed sores" is vital for any caregiver dealing with individuals at risk. By implementing preventive measures, recognizing early signs, and knowing treatment options, caregivers can significantly reduce the incidence of bed sores and improve the quality of life for those in their care. Education and vigilance are key to providing compassionate and effective care, ensuring that your loved ones remain comfortable and healthy.