As individuals approach "end-of-life care", the use of "antibiotics" often becomes a crucial consideration for both patients and healthcare providers. Understanding the role of antibiotics in this stage of life is essential for ensuring comfort and quality of care. This article provides valuable insights into "antibiotic use", the potential benefits, and the ethical considerations involved when navigating end-of-life medication.
When dealing with serious infections in terminally ill patients, the decision to use antibiotics can be complex. Many healthcare professionals weigh the benefits of treating infections against the overall goals of care. It is important to recognize that while antibiotics can help manage infections, they may not always be appropriate in the context of end-of-life care. Here are some key points to consider:
1. "Quality of Life": The primary goal of end-of-life care is to maintain or improve the patient's quality of life. In some cases, antibiotic treatment may alleviate symptoms of infections, providing relief and enhancing comfort. However, in other situations, the side effects of antibiotics or the invasive nature of treatment may diminish the patient's quality of life.
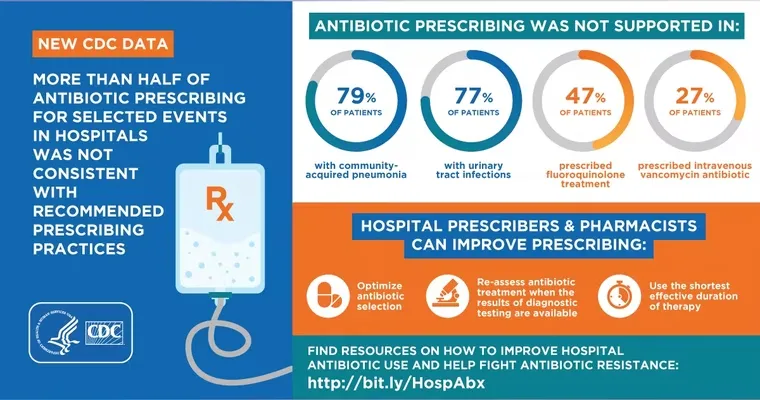
2. "Antibiotic Resistance": The overuse of antibiotics contributes to "antibiotic resistance", which is a significant concern in healthcare. When approaching end-of-life care, unnecessary prescriptions should be avoided to prevent further complications. It is crucial to assess whether the benefits of antibiotic treatment outweigh the risks of contributing to resistance.
3. "Patient Preferences": Engaging in open discussions with patients and their families about their wishes regarding antibiotic use is vital. Some patients may prefer to avoid aggressive treatments in favor of comfort measures, while others may wish to pursue all available options to fight infections. Understanding and respecting these preferences is key to providing compassionate care.
4. "Informed Decision-Making": Healthcare providers should offer clear information about the potential outcomes of antibiotic treatment, including the likelihood of recovery and the possible side effects. This allows patients and their families to make informed decisions that align with their values and goals.
5. "Palliative Care Approach": In many cases, a "palliative care" approach may be appropriate when managing infections in patients at the end of life. This approach focuses on relieving symptoms and improving the patient's overall comfort rather than aggressively treating infections. Palliative care teams can provide guidance on when antibiotics may be helpful and when they may not be necessary.
In conclusion, the use of antibiotics in end-of-life care requires careful consideration of the patient's condition, preferences, and the overarching goal of maintaining comfort. Engaging in thoughtful discussions among healthcare providers, patients, and families can lead to better outcomes and a more compassionate approach to care. As we navigate the complexities of "end-of-life medication", it is essential to prioritize the patient's well-being and make choices that honor their wishes.