Clostridioides difficile, commonly known as "C-diff", is a bacterial infection that can cause severe diarrhea and other intestinal issues. For many patients, traditional treatment methods like antibiotics may not be effective, leading to a growing interest in "C-diff experimental treatments". These innovative approaches are being researched to provide new solutions for individuals suffering from this challenging condition. In this article, we will explore the latest advancements in experimental treatments for C-diff and their potential benefits.
Understanding C-diff and Its Challenges
C-diff infections often occur after the use of antibiotics, which can disrupt the balance of good bacteria in the gut. The symptoms can range from mild diarrhea to life-threatening colitis. Recurrence is a significant concern, with many patients experiencing multiple episodes, making effective treatment essential. As the medical community seeks to address this issue, experimental treatments are being developed to offer alternative solutions.
The Role of Fecal Microbiota Transplantation
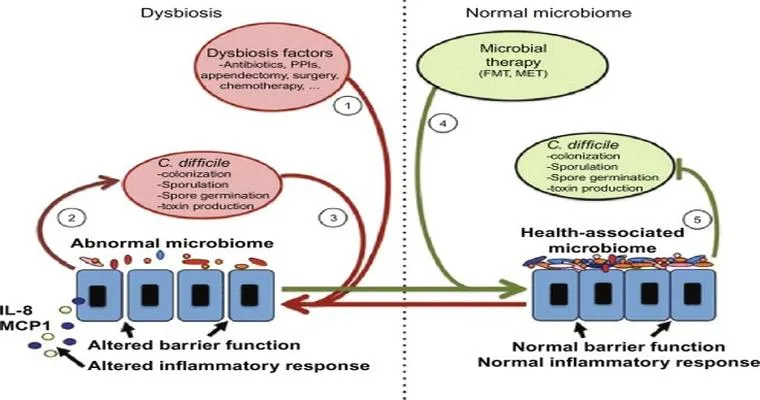
One of the most promising "experimental treatments" for C-diff is "fecal microbiota transplantation (FMT)". This procedure involves transferring stool from a healthy donor into the intestines of a C-diff patient. The goal is to restore the natural balance of gut bacteria, which can help eliminate the infection. Studies have shown that FMT can lead to high rates of cure for recurrent C-diff infections, making it a potential game-changer in the treatment landscape.
New Drug Developments
In addition to FMT, researchers are also exploring new "drug treatments" targeting C-diff. Several novel compounds are in various stages of clinical trials, aiming to inhibit C-diff toxins or disrupt its growth without harming beneficial gut flora. These drugs could provide more targeted therapy options, reducing the risk of recurrence and improving patient outcomes.
The Promise of Monoclonal Antibodies
Another exciting area of research involves the use of "monoclonal antibodies". These lab-produced molecules can target specific components of the C-diff bacteria or their toxins, neutralizing their harmful effects. Clinical trials are underway to assess the efficacy and safety of these treatments, and early results are promising. If successful, monoclonal antibodies could become a vital part of the C-diff treatment arsenal.
Future Directions in C-diff Treatment
As the understanding of C-diff infection evolves, so does the approach to treatment. Ongoing research into the "microbiome", the community of microorganisms living in the gut, is shedding light on how we can leverage these organisms to combat C-diff. Personalized medicine approaches, which tailor treatments based on an individual's microbiome profile, may offer the next frontier in C-diff management.
Conclusion
The landscape of C-diff treatment is rapidly changing, with "experimental treatments" offering new hope for patients. From fecal microbiota transplantation to novel drug therapies and monoclonal antibodies, these advancements could significantly improve the quality of life for those affected by C-diff infections. As research continues, it is essential for patients and healthcare providers to stay informed about these developments, ensuring access to the latest and most effective treatment options.