Delirium in dying is a critical aspect of end-of-life care that often goes overlooked. Many families and caregivers may not fully understand what "delirium" is, how it manifests during the "dying process", and the implications it has for the patient and their loved ones. This article aims to shed light on delirium, providing insights into its causes, symptoms, and management, ensuring that caregivers are better equipped to support those facing this challenging experience.
Delirium is a sudden change in mental status characterized by confusion, disorientation, and fluctuations in attention. It can occur in patients who are nearing death due to various underlying conditions, including severe illness, medication side effects, or metabolic imbalances. Understanding the "symptoms of delirium" is essential for identifying and addressing this condition promptly. Common signs include agitation, hallucinations, difficulty focusing, and altered sleep patterns.
One significant factor contributing to delirium in dying patients is the physiological changes that occur as the body begins to shut down. As organ function declines, the brain may not receive adequate oxygen and nutrients, leading to cognitive disturbances. Additionally, the use of certain medications, particularly opioids and sedatives, can exacerbate delirium symptoms.
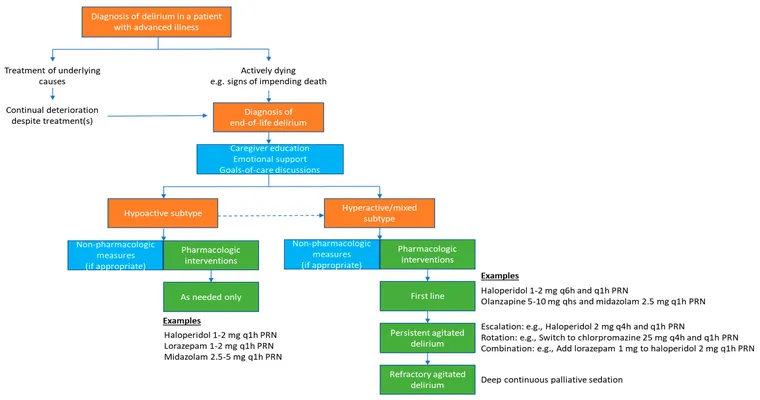
Caregivers and healthcare professionals must recognize the importance of proper assessment and intervention when dealing with delirium. A thorough evaluation should include a review of the patient’s medical history, current medications, and potential triggers for delirium. By identifying the root cause, appropriate measures can be taken to alleviate symptoms and enhance the patient’s comfort.
Management of delirium can vary depending on its severity and underlying causes. Non-pharmacological interventions, such as creating a calm environment, ensuring proper hydration and nutrition, and engaging the patient with familiar voices or music, can be beneficial. In some cases, medications may be necessary to manage severe agitation or distress, but these should be used judiciously and with careful consideration of the patient’s overall condition.
It is also crucial for families to understand the emotional and psychological impact of delirium. Patients may experience fear, confusion, and distress, which can be distressing for both the individual and their loved ones. Providing emotional support, maintaining open lines of communication, and offering reassurance can significantly improve the experience for everyone involved.
In conclusion, understanding "delirium in dying" is vital for providing compassionate and effective end-of-life care. By recognizing the symptoms, causes, and management strategies, caregivers can help ensure that patients experience a more peaceful and dignified transition. Education and awareness about delirium will not only improve the quality of care but also foster a supportive environment for both patients and their families during this challenging time.