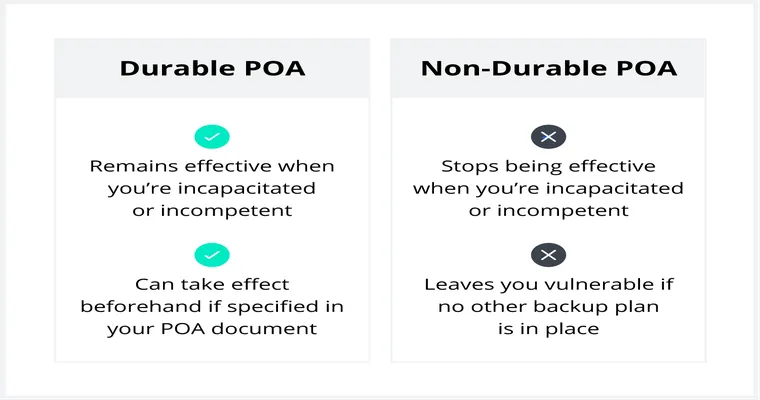
When dealing with the complexities of healthcare decisions, it's essential to understand the implications of a "medical power of attorney (POA)", especially for those navigating the emotional landscape of loss. My husband, who passed away, established a "medical POA" in 2013 and updated it in 2016 to reflect his wishes regarding end-of-life care. This included a "Do Not Resuscitate (DNR)" order, as well as a clear directive against "intubation" and the use of a "feeding tube". Understanding these documents can provide clarity during challenging times and ensure that a person's wishes are honored.
A "medical power of attorney" allows individuals to appoint someone to make healthcare decisions on their behalf if they become unable to do so. This legal document is crucial for ensuring that the person’s healthcare preferences are respected. In my husband's case, the updates made in 2016 were particularly important as they outlined his specific wishes regarding life-sustaining treatments.
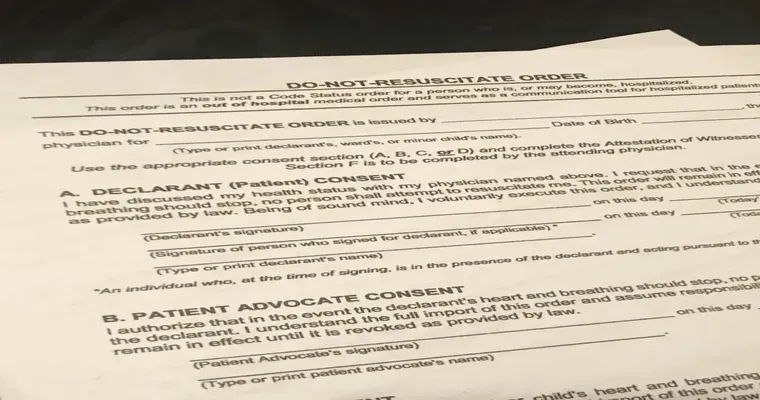
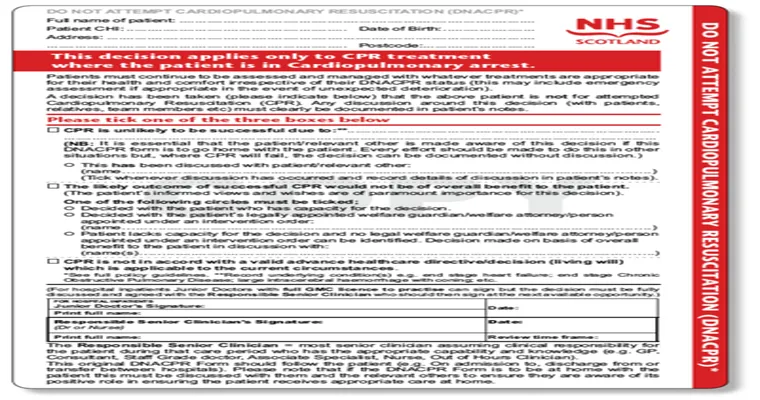
The inclusion of a "DNR" order indicates that he did not want resuscitation efforts in the event of cardiac arrest. This decision is often made after careful consideration and discussions with healthcare providers and loved ones. It reflects a person's wishes for a natural end-of-life process without aggressive medical interventions.
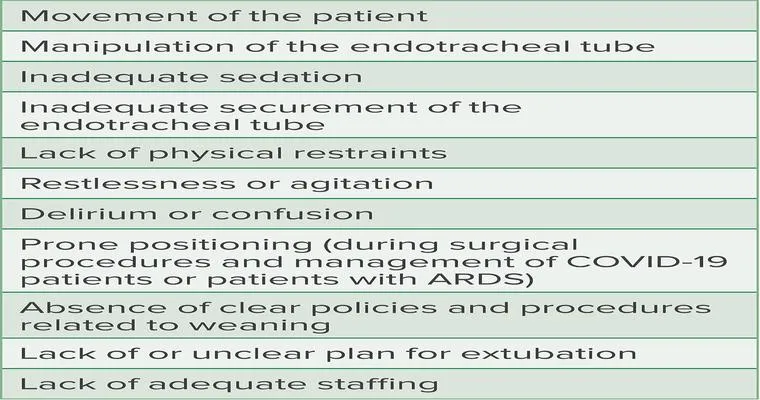
In addition to the "DNR", the directives against "intubation" and the use of a "feeding tube" further clarify his stance on life support measures. Intubation is often performed to assist with breathing, while a feeding tube provides nutrition when a person cannot eat. Both interventions can significantly alter the course of a person's final days, sometimes prolonging suffering rather than enhancing quality of life.
Navigating these decisions can be incredibly difficult, especially when faced with the emotional weight of losing a loved one. Having a "medical POA", along with clear directives like a "DNR" and specific treatment preferences, can alleviate some of that burden. It provides a roadmap for family members and healthcare providers, ensuring that the individual's wishes are not only known but respected.
It's beneficial for everyone to discuss these topics with their loved ones, even if they seem uncomfortable. Open conversations about healthcare preferences and the importance of having a "medical POA" can lead to better understanding and peace of mind for all parties involved.
In conclusion, understanding the nuances of a "medical power of attorney", including end-of-life directives like a "DNR", and preferences against "intubation" and "feeding tubes", can significantly aid in honoring a loved one's wishes. These documents serve as essential tools in ensuring that healthcare decisions align with the values and desires of the individual, providing clarity and comfort during times of uncertainty.