A "Do-Not-Resuscitate (DNR) order" is a legal document that allows individuals to refuse specific medical interventions, particularly CPR, in the event of cardiac arrest or respiratory failure. This order is crucial for patients who wish to avoid aggressive life-saving measures that may not align with their personal values or quality of life considerations. Understanding what a DNR order entails and how it operates is essential for both patients and their families.
Understanding a Do-Not-Resuscitate Order
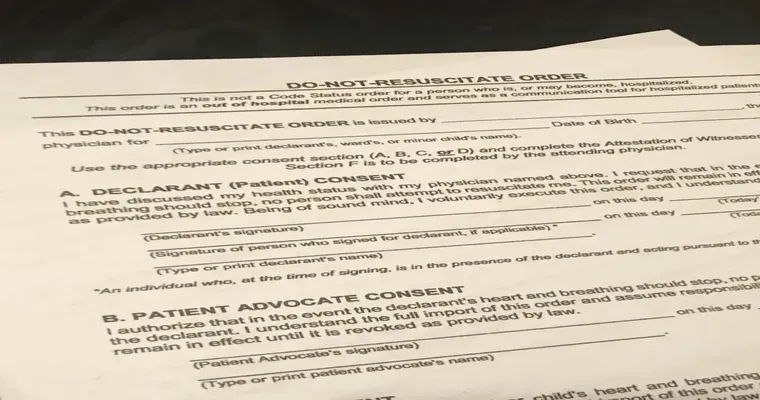
A DNR order is typically issued by a physician and is often part of an individual's broader advance care planning. This planning involves discussions about future healthcare preferences and decisions, especially for those with terminal illnesses or severe medical conditions. The DNR specifically instructs healthcare providers not to perform CPR or other resuscitation efforts if the patient's heart stops beating or if they stop breathing.
Who Should Consider a DNR Order
DNR orders are not just for elderly patients or those in hospice care. Any individual facing a serious health condition or those who have strong preferences about end-of-life care may consider a DNR. It is important for patients to have open discussions with their families and healthcare providers about their wishes regarding resuscitation efforts.
How to Obtain a Do-Not-Resuscitate Order
To obtain a DNR order, an individual typically needs to discuss their wishes with a healthcare provider. The process generally involves the following steps:
1. "Consultation with a Doctor": The patient should have a detailed conversation with their physician about their health status and treatment preferences.
2. "Completion of the DNR Form": If both parties agree, the physician will help the patient complete a DNR form. This form should include the patient's name, medical condition, and a clear statement of their wish not to receive CPR.
3. "Signature and Documentation": The DNR order must be signed by both the patient (or their legal representative) and the physician. It is essential to keep copies of this document in a place accessible to healthcare providers.
4. "Communication with Family": Patients should inform their family members about the DNR order to ensure everyone is aware of their wishes.
The Role of Healthcare Providers
Healthcare providers play a significant role in respecting and implementing DNR orders. When a DNR is in place, medical teams must adhere to the patient's wishes and provide appropriate end-of-life care without aggressive interventions. It is crucial for healthcare providers to have access to the DNR documentation to act accordingly in emergencies.
Legal Considerations and Variations
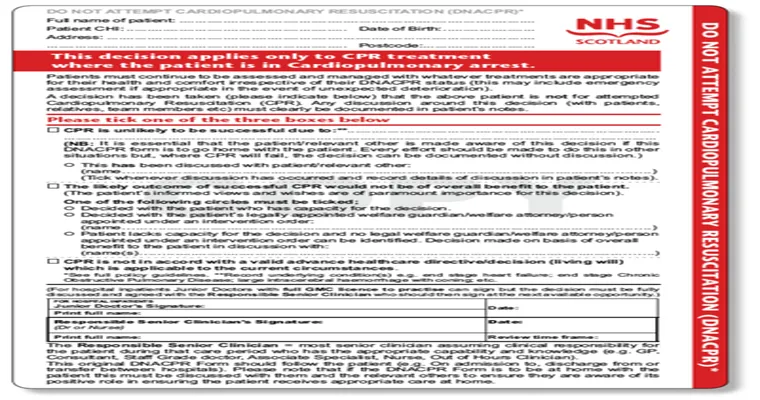
DNR orders can vary by state or country, and it is important for individuals to understand their local laws regarding these directives. Some regions may have specific forms or additional requirements for a DNR to be valid. Therefore, consulting with a legal expert or a healthcare professional familiar with local regulations can be beneficial.
Conclusion
A "Do-Not-Resuscitate order" is an important aspect of advance care planning for individuals who wish to dictate their end-of-life medical treatment. By understanding how a DNR works and the steps required to obtain one, patients can ensure that their healthcare preferences are honored. Open communication with healthcare providers and family members is essential for making informed decisions that align with personal values and wishes.