"Pre-diabetes" is a crucial health condition that affects millions of people worldwide. It serves as a warning sign that your blood sugar levels are elevated but not yet high enough to be classified as "type 2 diabetes". Understanding pre-diabetes is essential for preventing the progression to diabetes and reducing the risk of serious health complications. In this article, we will explore what pre-diabetes is, its risk factors, symptoms, and effective management strategies.
What is Pre-Diabetes?
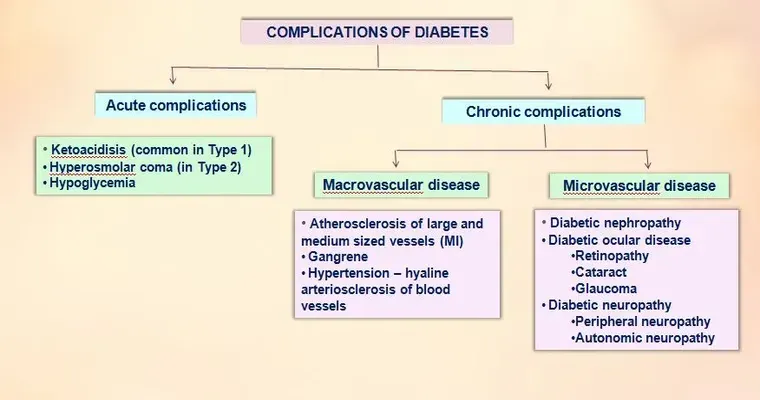
Pre-diabetes occurs when your blood glucose levels are higher than normal but not high enough to be diagnosed as diabetes. This condition indicates that your body is beginning to struggle with insulin sensitivity, which is vital for regulating blood sugar levels. If left unaddressed, pre-diabetes can lead to "type 2 diabetes", heart disease, and other serious health issues.
Risk Factors for Pre-Diabetes
Several factors can increase your likelihood of developing pre-diabetes. These include:
"Being overweight": Excess weight, especially around the abdomen, significantly raises the risk.
"Age": Individuals over the age of 45 are at a higher risk.
"Family history": A family history of diabetes can increase your susceptibility.
"Sedentary lifestyle": Lack of physical activity contributes to weight gain and insulin resistance.
"Unhealthy diet": A diet high in processed foods, sugars, and unhealthy fats can increase blood sugar levels.
Symptoms of Pre-Diabetes
Many people with pre-diabetes do not experience noticeable symptoms. However, some may exhibit signs such as:
Increased thirst
Frequent urination
Fatigue
Blurred vision
Dark patches of skin, particularly around the neck and armpits
If you notice any of these symptoms, it is essential to consult a healthcare professional for testing.
Diagnosis of Pre-Diabetes
Diagnosis is typically made through blood tests. The most common tests include:
"Fasting blood sugar test": Measures your blood sugar levels after an overnight fast.
"Oral glucose tolerance test": Measures blood sugar levels before and two hours after consuming a sugary drink.
"Hemoglobin A1c test": Provides an average blood sugar level over the past two to three months.
A fasting blood sugar level of 100 to 125 mg/dL, an A1c of 5.7% to 6.4%, or a two-hour glucose level of 140 to 199 mg/dL indicates pre-diabetes.
Managing Pre-Diabetes
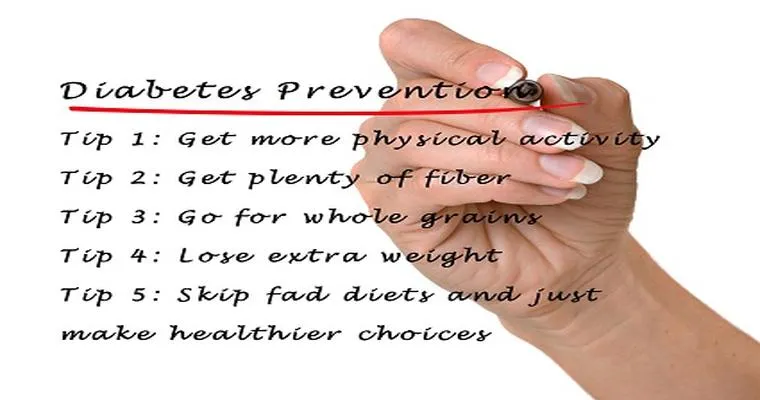
The good news is that pre-diabetes is reversible. Here are some effective strategies to manage and potentially reverse the condition:
1. "Healthy Eating": Focus on a balanced diet rich in whole grains, lean proteins, fruits, and vegetables while minimizing refined carbs and sugars.
2. "Regular Exercise": Aim for at least 150 minutes of moderate aerobic activity each week, such as brisk walking or cycling.
3. "Weight Loss": Losing even a small percentage of body weight can significantly reduce the risk of developing diabetes.
4. "Regular Monitoring": Keep track of your blood sugar levels and have regular check-ups with your healthcare provider.
5. "Education": Learn about pre-diabetes and diabetes management to make informed decisions about your health.
Conclusion
Understanding pre-diabetes is the first step toward preventing its progression to type 2 diabetes. By recognizing the risk factors, symptoms, and management strategies, you can take control of your health. If you suspect you may have pre-diabetes, consult your healthcare provider for testing and guidance. Remember, early intervention is key in transforming your health and reducing the risk of serious complications.