In today's healthcare landscape, the decision to decline "life-prolonging treatment" is increasingly becoming a significant topic of discussion. Patients, families, and healthcare providers are grappling with the implications of such choices, which can often lead to "blocked exits" in the continuum of care. Understanding the nuances of this decision-making process is essential for ensuring that patients receive the most appropriate and compassionate care.
The choice to decline life-prolonging treatment can stem from various factors, including the quality of life considerations, the severity of the illness, and personal values. Many patients find themselves at a crossroads, weighing the benefits of aggressive treatment against the potential for prolonged suffering. This is particularly relevant in cases of terminal illnesses where the prognosis is poor, and the likelihood of recovery is minimal. In such situations, the emphasis often shifts from extending life to improving "quality of life".
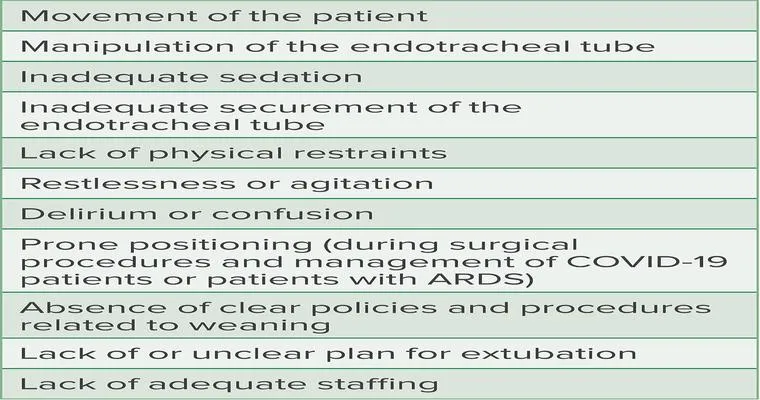
When patients choose to decline life-prolonging treatment, they may inadvertently create "blocked exits" in their care journey. This term refers to the barriers that arise when the healthcare system is not adequately prepared to support patients who opt for less aggressive interventions. For instance, if healthcare providers do not have clear communication with patients about their choices and preferences, it can lead to misunderstandings and conflicts regarding care plans. This lack of clarity can result in patients receiving unwanted treatments or interventions that do not align with their wishes.
To prevent these blocked exits, it is crucial for healthcare providers to engage in open and honest discussions with patients about their treatment options. This includes exploring the potential benefits and drawbacks of life-prolonging treatments, as well as discussing alternative approaches that prioritize comfort and dignity. Enabling patients to express their values and preferences can lead to more personalized care plans that align with their goals.
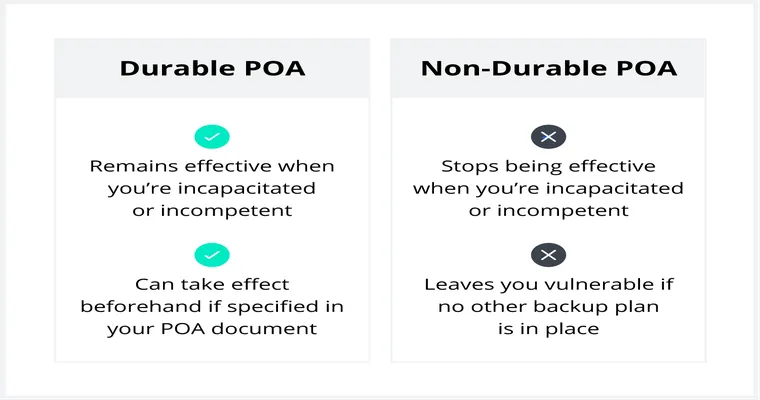
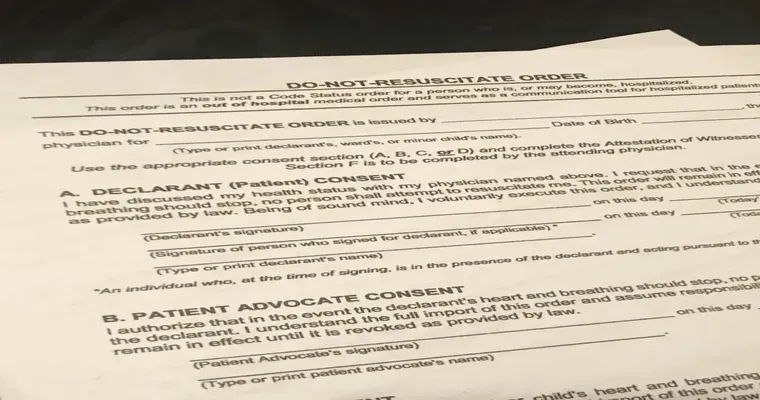
Moreover, advance care planning plays a vital role in addressing the complexities of declining life-prolonging treatment. Encouraging patients to articulate their wishes through advance directives can help ensure that their preferences are respected, even when they may no longer be able to communicate them. This proactive approach can significantly reduce the likelihood of blocked exits by providing a clear framework for decision-making that reflects the patient's values.
In conclusion, the decision to decline life-prolonging treatment is a deeply personal one that requires careful consideration of various factors. By fostering open communication and supporting advance care planning, healthcare providers can help patients navigate this challenging process. Ultimately, the goal should be to create a healthcare environment that respects patient choices and minimizes blocked exits, allowing individuals to receive care that truly aligns with their wishes and enhances their quality of life.