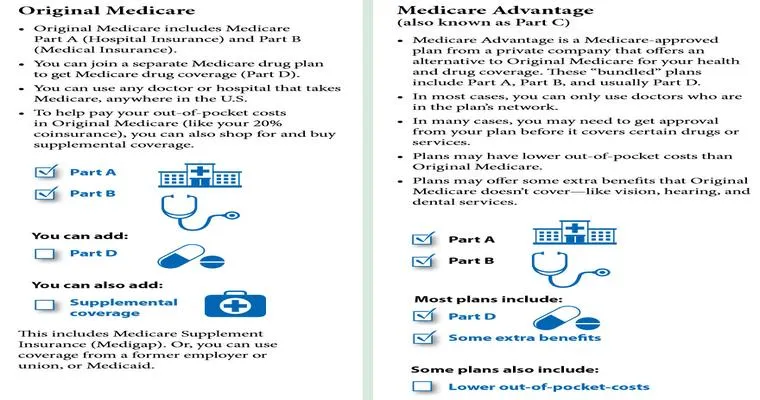
When it comes to "Medicare" and "Anthem" coverage, understanding the guidelines for "Schedule A benefits" is crucial, especially after a loved one has utilized nursing home services. In this article, we will explore the specifics surrounding the reinstatement of Schedule A benefits after your mother has received "100 days of nursing home care" funded by these programs.
Understanding Medicare's Coverage for Nursing Homes
Medicare Part A typically covers a stay in a skilled nursing facility for a limited time. Generally, this coverage can extend up to "100 days" if certain conditions are met. For your mother to qualify for this extended coverage, she must have been admitted to the nursing home following a "three-day inpatient hospital stay" and require skilled care that cannot be provided at home.
Guidelines for Reinstatement of Schedule A Benefits
If your mother has used her full 100 days of nursing home care, you might be wondering how to get her Schedule A benefits reinstated. Here are the essential guidelines to consider:
1. "Review Eligibility Requirements": To qualify for Medicare coverage again, your mother must meet the eligibility criteria, which include being hospitalized for at least three consecutive days and needing skilled nursing care. If she has not been hospitalized since her nursing home stay, she may not qualify for reinstatement.
2. "Skilled Care Needs": For her benefits to be reinstated, your mother must demonstrate a need for skilled nursing services. This may include physical therapy, occupational therapy, or other medically necessary treatments. A physician's evaluation can help determine her current care needs.
3. "Waiting Period": After using 100 days of skilled nursing care, there is typically a waiting period before Medicare benefits can be reinstated. In many cases, this may involve a new hospital stay or a break in skilled nursing services for a certain period, often 60 days. It is essential to confirm the specific waiting period with Medicare or Anthem.
4. "Appeal Process": If you believe that benefits were denied in error or if her condition has changed significantly, you can appeal the decision. Gather all necessary documentation, including medical records and care plans, to support your case.
5. "Consulting Healthcare Professionals": Engaging with healthcare professionals, including social workers and case managers at the nursing facility, can provide valuable insights into your mother's care needs and the necessary steps to reinstate her coverage.
6. "Regular Assessments": Schedule regular assessments with her healthcare team to ensure that her needs are being met and to evaluate her eligibility for further nursing home care under Medicare.
Conclusion
Navigating the complexities of "Medicare" and "Anthem" benefits can be challenging, especially after a loved one has utilized skilled nursing services. Understanding the guidelines for reinstating Schedule A benefits is essential for ensuring that your mother receives the care she needs. By staying informed about eligibility requirements, skilled care needs, and the appeal process, you can effectively manage her healthcare and make the best decisions for her well-being. Always consult with healthcare professionals and refer to official Medicare resources for the most accurate and up-to-date information regarding your mother's coverage.