In the realm of "senior care", particularly for those with a "Do Not Resuscitate (DNR)" order, the decision to administer "appetite enhancing drugs" and "antidepressants" raises significant ethical and medical considerations. As caregivers and healthcare professionals navigate the complexities of end-of-life care, understanding the implications of these treatments is essential.
When a senior individual with a DNR status is no longer eating or walking, it often signals a decline in health and quality of life. This situation can be distressing for families and caregivers, prompting questions about the appropriateness of continuing to administer medications aimed at improving appetite and mood.
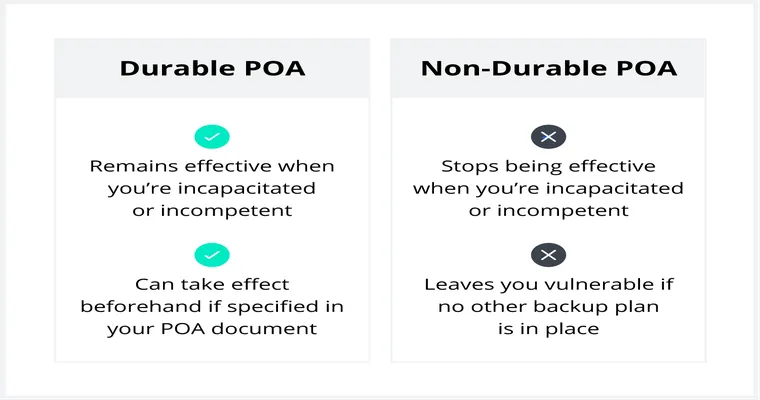
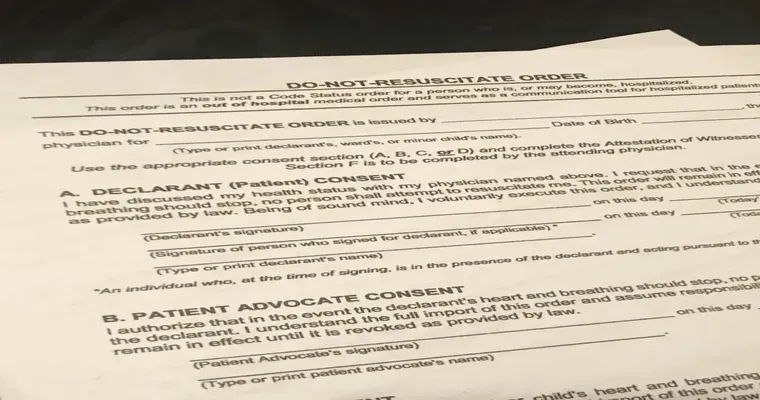
Understanding DNR Orders
A DNR order is a legal document that indicates a patient's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. This order is typically established when a patient is nearing the end of life or has a terminal illness. The focus of care shifts to maintaining comfort rather than prolonging life through aggressive medical interventions.
The Role of Appetite Enhancing Drugs
Appetite enhancing drugs, such as "megestrol acetate" or "mirtazapine", may be prescribed to seniors who are experiencing weight loss or decreased desire to eat. These medications can stimulate appetite, potentially improving nutritional intake. However, the decision to use these drugs in a patient with a DNR status requires careful consideration.
For many seniors, the natural progression of their condition may lead to a decreased desire to eat. In such cases, force-feeding or aggressively trying to enhance appetite could lead to discomfort or distress. Therefore, it is crucial to assess whether the goals of care align with the patient's wishes and overall health status.
The Use of Antidepressants
Similarly, the use of antidepressants may be considered for seniors experiencing depression, which can often accompany chronic illness or terminal conditions. Medications like "sertraline" or "escitalopram" may help lift mood and improve quality of life. However, the appropriateness of these medications in the context of a DNR order must be evaluated.
Antidepressants can have side effects that might complicate a patient's condition, especially in advanced stages of illness. Additionally, the potential benefits must be weighed against the patient's current state and their expressed desires regarding treatment.
Ethical Considerations
The ethical considerations surrounding the use of appetite enhancers and antidepressants in seniors with a DNR status are multifaceted. Healthcare providers must engage in open dialogues with patients and their families to ensure that treatment aligns with the patient's values and wishes.
Decisions should be guided by principles of "beneficence" (acting in the best interest of the patient), "non-maleficence" (avoiding harm), and "autonomy" (respecting the patient's right to make informed choices about their care). A palliative care approach may be appropriate, focusing on comfort and quality of life rather than aggressive treatment.
Conclusion
In conclusion, the administration of appetite enhancing drugs and antidepressants to a senior with a DNR status who is not eating or walking requires a thoughtful, patient-centered approach. Caregivers and healthcare professionals must carefully consider the ethical implications, the patient's quality of life, and their expressed wishes. By doing so, they can provide compassionate care that honors the dignity and autonomy of the individual, ultimately enhancing their well-being in their final days.