
Selected reviews about elderly care communities
Selected reviews about elderly care communities offer valuable insights into the experiences of residents and their families. These reviews can highlight the strengths and weaknesses of different communities, helping you make an informed decision when choosing the right care for your loved one.

My niece has a POA for my Mom. Can doctors withhold information?
When a niece holds power of attorney for her mother, she typically has the right to access medical information. However, doctors may withhold information if they believe disclosing it could harm the patient’s health or well-being. It's essential to understand the legal boundaries surrounding medical privacy and consent.

How can I find information on aide care?
To find information on aide care, explore online resources like government health websites, local healthcare providers, and community organizations. Consider reaching out to support groups or forums for personal experiences and recommendations. Additionally, consult professionals in the healthcare field for guidance on available services and options tailored to your needs.

Is it legal for the caregiver company to tell us we can't have a camera in her bedroom while she is changed?
The legality of a caregiver company prohibiting cameras in a client's bedroom during personal care often hinges on privacy rights and consent. Caregivers may enforce such policies to protect the dignity and confidentiality of their clients, but it's essential to review the specific regulations and agreements in place regarding monitoring and privacy.
Do I (POA) have legal rights to view medication given by a memory care facility? This is in California.
In California, a Power of Attorney (POA) typically grants the authority to make healthcare decisions on behalf of an individual. This includes the right to access medical records and information about medications administered in a memory care facility, ensuring informed decisions regarding the individual's care and treatment.

A step-family member was granted conservatorship and guardianship to my stepmother. Can he/she answer my stepmother's health status questions?
A step-family member granted conservatorship and guardianship over your stepmother can make decisions regarding her health and well-being. This role typically includes the authority to obtain and respond to inquiries about her health status, ensuring her medical needs are met and her best interests are prioritized.
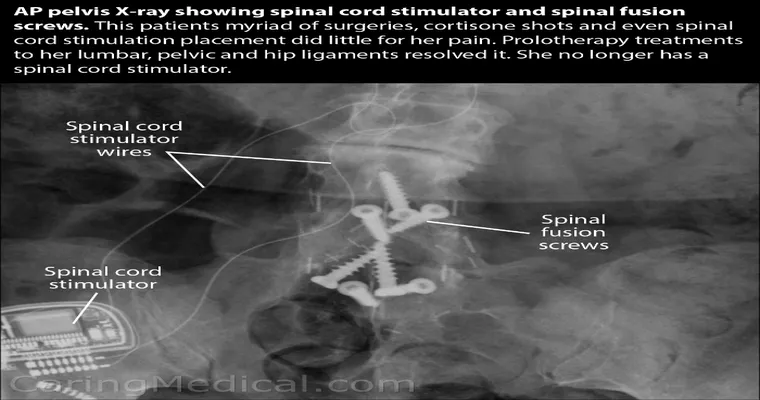
My husband is partially disabled from 4 back surgeries, a total hip and soon another hip surgery. In Gr8 pain and has begun using alcohol. Ideas?
My husband struggles with chronic pain due to multiple surgeries and is increasingly relying on alcohol for relief. This situation is affecting both his physical and mental health, and I’m seeking effective strategies to support him through this challenging time, while also addressing his dependence on alcohol.

The form was a bit misleading. I'm the patient, my oldest son is a part-time caregiver when he is home. Now I can only take a few steps.
The form's wording caused some confusion regarding my situation. As the patient, I rely on my oldest son, who is a part-time caregiver when he is home. Currently, my mobility is limited, and I can only manage to take a few steps, making daily tasks increasingly challenging.

99-year-old mom with dementia broke her hip. Opinions?
A 99-year-old mother with dementia recently suffered a hip fracture, raising concerns about her care and quality of life. Opinions vary on the best approach to her recovery, balancing the need for medical intervention with the potential stress of rehabilitation. Families grapple with emotional and ethical dilemmas in such situations.
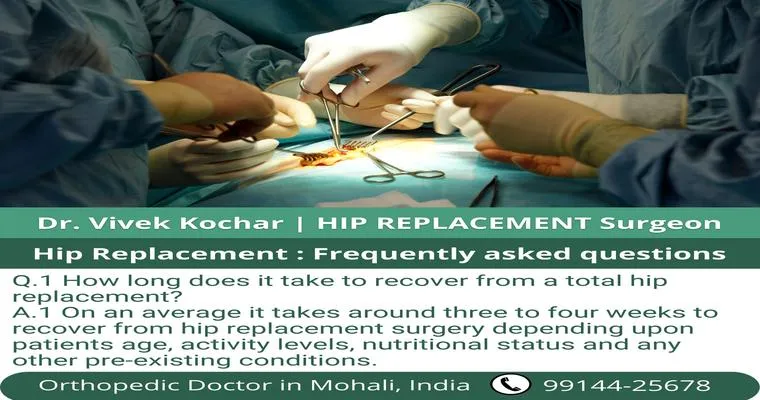
Hip replacement questions.
Hip replacement questions often revolve around the procedure's purpose, recovery time, potential risks, and long-term outcomes. Patients frequently inquire about the best candidates for surgery, the materials used in implants, and the impact on mobility and pain relief. Understanding these aspects can help in making informed decisions about treatment options.

My mom just died 81 yrs. old. She fell broke her hip, Dr.'s did hip replacement but 3 days later she suffered a massive stroke and went into a coma.
My mom, at 81, faced a tragic turn after breaking her hip. Despite undergoing surgery for a hip replacement, she suffered a massive stroke just three days later and slipped into a coma. Her sudden loss leaves a profound void, and I cherish the memories we shared.
I’m miserable in my marriage and want to leave, but my husband needs a hip replacement. Would It be awful to leave him now?
Feeling trapped in a difficult marriage while facing your husband's impending hip replacement creates a profound emotional conflict. You grapple with the desire for personal happiness against the fear of abandoning him during a vulnerable time. This dilemma raises questions about compassion, responsibility, and the right moment to prioritize your own well-being.
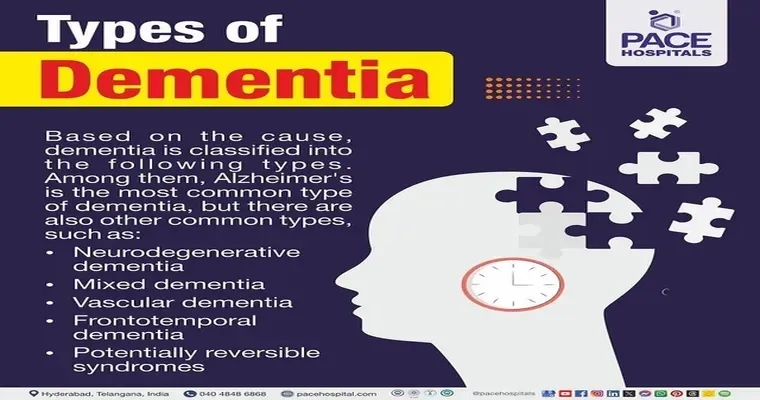
Dementia with Behavioral Disturbances: Behaviors, Causes, and Types
Dementia with behavioral disturbances encompasses various psychological symptoms that can manifest in individuals with dementia. These behaviors may include aggression, agitation, and mood swings, often stemming from underlying cognitive decline, anxiety, or environmental triggers. Understanding the types and causes is crucial for effective management and improving the quality of life for affected individuals.
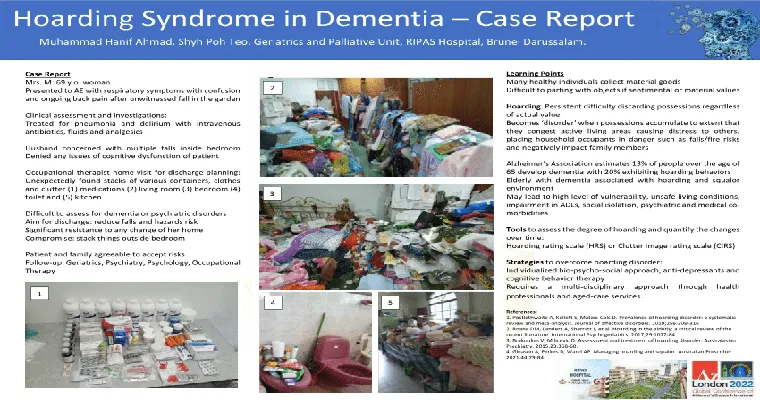
Hoarding: A Challenging and Potentially Dangerous Dementia-Related Behavior
Hoarding is a complex behavior often associated with dementia, where individuals accumulate excessive items, leading to cluttered living spaces. This behavior can pose significant safety risks, impede daily functioning, and create emotional distress for both the individual and their caregivers. Understanding and addressing hoarding is crucial for effective dementia care.

How Do I Get Dad Out of His Cluttered, Unsafe Home?
To help Dad leave his cluttered, unsafe home, start by having an open conversation about his living conditions. Offer to assist with sorting and decluttering, emphasizing safety and comfort. Explore alternative living arrangements, such as assisted living or moving in with family, ensuring he feels supported and involved in the decision-making process.

Dangers of Hoarding Behavior Become More Severe With Age
Hoarding behavior can intensify with age, leading to increased clutter and safety hazards in living spaces. Older adults may struggle with decision-making and emotional attachment to possessions, resulting in isolation and health risks. Addressing these issues early is crucial to improve well-being and maintain a safe environment for aging individuals.

Does HIPPA protect the LO's privacy but hinder them from getting the treatment that they not only need but deserve?
HIPAA safeguards the privacy of individuals' health information, ensuring confidentiality. However, this strict protection can sometimes create barriers for loan originators in accessing necessary treatment. The balance between maintaining privacy and enabling access to care can complicate their ability to receive the support they need and deserve.
Why I feel HIPPA is outdated. When there are too many secrets going around, people cannot get the care they need...
HIPAA feels outdated because its strict privacy regulations can hinder patient care. When too much emphasis is placed on confidentiality, vital information may be withheld, preventing healthcare providers from delivering appropriate treatment. This creates barriers that ultimately compromise the quality of care patients receive in critical situations.

Preparing a Senior with Dementia for a Doctor's Visit
Preparing a senior with dementia for a doctor's visit involves creating a calm environment, providing clear information about the appointment, and using familiar objects or photos to reduce anxiety. It's important to involve caregivers, ensure timely transportation, and maintain a reassuring presence throughout the visit to enhance comfort and understanding.
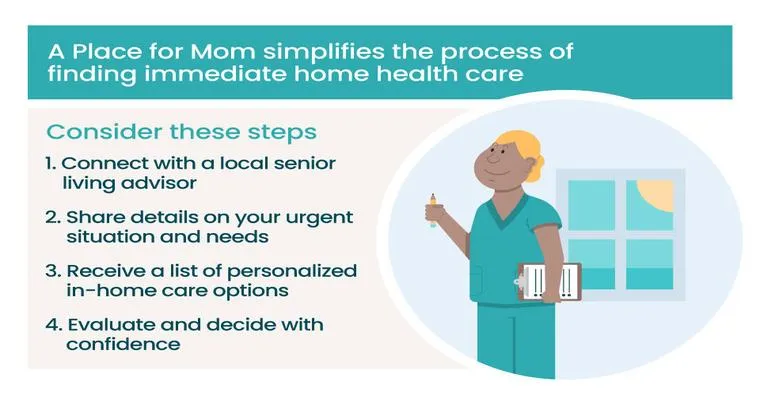
First Steps for New Caregivers: Getting a Health Assessment for Your Parent
New caregivers face the crucial task of obtaining a health assessment for their parent. This process involves understanding their medical history, evaluating current health conditions, and identifying specific needs. Engaging healthcare professionals ensures a comprehensive approach, enabling caregivers to provide appropriate support and make informed decisions for their loved one's well-being.

How HIPAA Impacts Caring for Aging Parents
HIPAA significantly influences the care of aging parents by protecting their medical information while ensuring family members can access necessary health details. Understanding these privacy regulations is crucial for caregivers, as it helps navigate consent and communication with healthcare providers, ultimately enhancing the support and quality of care for aging loved ones.
Page 61 of 134